
It is my belief that an excellent postoperative patient result begins with detailed attention to preoperative testing. With its diverse pre- and postoperative evaluation capabilities, the OPD-Scan III has improved my surgical outcomes and has increased overall patient satisfaction. Furthermore, I use the images on the OPD to discuss diagnoses and treatment plans with patients.
Pre-op Screening for Optimal Post-op Results
To achieve the best postoperative results, we must screen patients preoperatively to identify certain corneal disorders that may affect outcomes. The OPD-Scan III measures a large amount of data, all of which are helpful in determining the best treatment options for patients. We are constantly finding new ways to maximize its advantages. The OPD has led to reduced postoperative issues and complaints by helping me to properly select those patients who would be good candidates for premium IOLs.
For example, the OPD identifies corneal diseases — such as irregular astigmatism, higher-order aberrations (corneal coma or corneal trefoil), high or low spherical aberration, and visually significant pterygiums with irregular astigmatism extending into the central pupillary zone. In each of these situations, the patient would be considered a poor candidate for a multifocal IOL.
I also evaluate the placido rings to look for irregularities. Irregular placido rings can be caused by a wide variety of corneal diseases, including dry eye disease, pterygiums, keratoconus, Salzmann’s nodules, corneal scarring, and epithelial basement membrane disease. If I decide to treat the corneal disease prior to cataract surgery, I obtain a repeat scan after surgery to show patients the subsequent improvement in the placido rings. This helps demonstrate the benefits of having an additional surgery prior to cataract surgery.
The OPD is especially helpful for identifying subtleties of dry eye preoperatively that I may not have otherwise noticed. It is easily seen as irregular placido rings, which can be shown to patients for educational purposes. From there, we begin a more thorough dry eye evaluation. After treating the dry eye disease, I repeat the preoperative testing and IOL calculations. Always address dry eye disease before surgery.
In addition, I evaluate all patients who have had previous LASIK, PRK, or RK. I am looking for irregular astigmatism, high spherical aberration, or a decentered ablation. I discuss these findings with patients preoperatively, explaining that prior refractive surgery may affect their final postoperative result, and because of this, it is possible that not all glare or decreased contrast sensitivity problems will be resolved.
The OPD also measures corneal spherical aberration, which allows me to customize my choice of IOL to best correct it. This helps to optimize each patient’s postoperative visual outcome.
Pre-op Screening of Premium IOL Patients
The OPD is especially valuable when evaluating patients who are interested in a toric IOL. The axial map is useful in confirming the planned axis for the orientation of the toric IOL, which should be very similar to the axis obtained via optical biometry. If the axis from the axial map and optical biometry are not similar, I repeat testing and look for the previously mentioned corneal disorders.
The OPD-Scan III also assists me in the multifocal IOL decision-making process. When evaluating multifocal patients preoperatively, I look for corneal disease. In general, the more irregular the cornea, the less likely I would be to use a premium IOL. For example, if a patient has significant higher-order aberrations, I would not use a multifocal IOL. In addition, I evaluate the mesopic and photopic pupil size. If the mesopic pupil size is greater than 6 mm, I have a discussion with the patient about an increased risk for halos and glare postoperatively. However, if the patient has a small photopic pupil less than 3 mm, I generally use a multifocal IOL in which the near vision isn’t dependent on pupil size. I also use the OPD to evaluate angle kappa. If angle kappa is greater than .43 mm, I use a multifocal IOL with a larger central zone.
Consistent Results with Post-op Screening
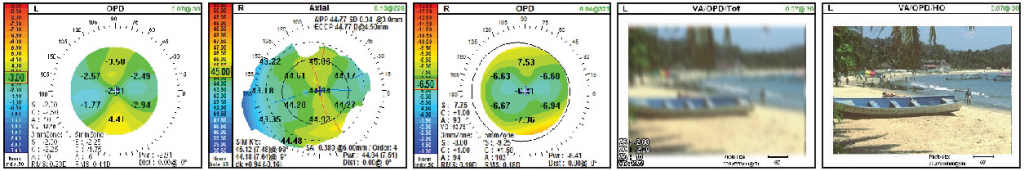
I obtain postoperative OPD-Scan III studies on all of my multifocal patients. Approximately 1 week after surgery, I obtain a dilated reading. This allows me to see if the central zone of the IOL is centered within the visual axis of the patient. If not, I know the IOL has shifted postoperatively, which frequently results in patient complaints of decreased vision and glare. Complaints usually can be resolved by surgically repositioning the multifocal IOL onto the visual axis.
I will also perform an OPD scan 1 week post-op on patients who received a toric IOL. Again, the scan is obtained with a dilated pupil. In this way, I can measure the axis orientation of the toric IOL to ensure that the toric IOL didn’t rotate away from the intended axis of surgical orientation. Correct toric alignment is critical because the power of the astigmatic correction is reduced 10% for every 3 degrees away from the intended axis of orientation. If there is significant rotation of the toric IOL, I will take the patient back to the OR to realign the toric IOL to the proper orientation.
More Information = Happier Patients
The OPD-Scan III has significantly reduced the number of post-op complaints from patients. With more information to guide me through the entire process, I’ve been able to largely avoid unhappy multifocal IOL patients by identifying the best candidates up front. Before we acquired the OPD, we were inconsistent when making these pre-op decisions.
Making the right decision as a surgeon is only one component of meeting or exceeding patient expectations. It’s also important that I educate patients at each step along the way. Pre-op tests help me manage expectations by educating patients with the aid of easy-to-understand test results. Visual aids help explain variables to improve patient understanding. For example, using OPD results, I can show a patient that his lens is well centered and his toric IOL is well positioned. Patients can see irregular placido rings consistent with dry eye syndrome, which reinforces the need to treat their dry eye prior to surgery.
Imaging can also show patients why irregular astigmatism may prevent them from being premium IOL candidates. With this information and education, patients better understand why you’re making certain decisions, they recognize that you’re trying to make the best decision for them — and they appreciate that.
Customization = Efficiency
The varied capabilities of the OPD allow us to create a specific map for pre- and post-op testing to meet the needs of each patient. We created a customized map to include all the important information we need to preoperatively evaluate the patient. By consolidating all the important measurements on one map, pre-op patient evaluations are much more efficient and allow us to create a personalized treatment plan for each patient. It’s amazing how many options there are with this instrument. We have customized it for our needs, and certainly other offices can adjust their maps to accommodate their needs as well.
We have also developed a comparison map to evaluate pre- and post-op LRI data to evaluate femtosecond laser LRI treatments. The outcome analysis can be used to adjust your LRI nomogram for any under-correction or over-correction of astigmatism. You may also use the comparison map to look for any increase or decrease in higher-order astigmatism, which may occur after an LRI.
Improve Satisfaction and Results
We acquired the OPD-Scan III about 5 years ago in an effort to improve our outcomes and patient satisfaction. It has delivered by helping us to preoperatively detect corneal issues that may affect outcomes, identify the best candidates for premium IOL surgery, improve surgical outcomes, and increase patient satisfaction.
– Dr. Ludwick specializes in cataract surgery and is the Medical Director at Ludwick Eye Center, with locations in Maryland and Pennsylvania. He is also an assistant clinical professor at Penn State Hershey Medical Center

